Healix™
Reliable, effective, accessible veterinary products
focused on animal health
The Biofactors
Epidermal Growth Factor (hEGF)
A diverse polypeptide whose synthesis and action is not restricted to defined tissues. Provides essential signaling to modify cell proliferation, maturation and migration. Accelerates wound healing and skin regeneration through promoting growth and division of epithelial and endothelial cells, stimulating fibroblast activity and keratinocyte migration.
Fibroblast Growth Factor (hbFGF)
Involved in the regulation of fundamental cellular processes and propagates effects through the fibroblast growth factor pathway. FGF plays a crucial role in wound healing, functioning to stimulate a range of cell types essential in protein and collagen synthesis, neovascularization and epithelialization. Activates keratinocytes, chondroblasts, myoblasts, capillary endothelial cells and promotes proliferation and migration of fibroblasts. Accelerates formation of granulation tissue, wound contraction and closure.
Utilizing exclusive Medical-grade Bio factors to create Innovative Veterinary Products
Superior bio factors hEGF and hbFGF were previously only available to limited hospitalized patients even in the human medical field due to their rarity and cost. Developments in bioengineering techniques now allows cultivation of high-quality growth factors shown to play an essential role in cellular regeneration and wound healing. Understanding the need for topical products to stimulate skin regeneration and to promote corneal ulcer repair, these high-purity bio factors have been incorporated into innovative veterinary products in the Healix range.

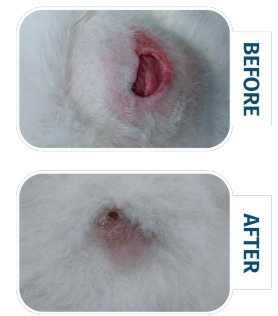
Skin Regenerating and Wound BioRepair
Healing of damaged skin is a complicated process which needs to progress through the stages of inflammation, debridement, repair and maturation. A variety of cell types are involved in the healing process and are naturally stimulated by growth factors which signal cells on the periphery of the wound to migrate and repair the skin defect with granulation tissue.
Fibroblasts are able to secrete collagen and elastin to create extracellular matrix which is the basis of granulation tissue.
Endothelial cells are activated at the site of the wound by angiogenic factors including fibroblast growth factor and allows the formation of new blood vessels.
Keratinocytes adjacent to the wound undergoes activation and proliferation, migrating across the wound to allow reepitheliaisation and epidermal repair. Keratinocytes produce signals to further activate more keratinocytes and other cell types, contributing to the fibroblast growth factor pathway and the formation of granulation tissue and differentiation of myofibroblasts.
Arising from fibroblasts which have successfully migrated across the wound bed to the center of the wound, myofibroblasts are responsible for contracting and drawing in the wound edges towards the center of the wound to allow wound closure. To achieve complete wound healing, the fragile newly-formed granulation tissue needs to remain moist and well-vascularized to support normal cell function and help epithelial cells to migrate.
Research has shown acceleration and improvement of wound healing through application of growth factors on dermal ulcers and wounds on rabbits. 1,2 A study on wound healing in hairless dogs showed that in comparison to the control, wounds treated with EGF “exhibited earlier re-epithelialization of the epidermis and highly regulated repair of extracellular matrix in the dermis”. 3 Delayed or incomplete wound healing presents as difficult challenges in patients under steroid treatment and a study on rats has shown that “EGF treatment can prevent the inhibitory effects of methylprednisolone on wound healing by stimulating fibroblast proliferation”.4
In chronic non-healing wounds, cell signaling is deficient and essential cell types are not able to undergo proliferation and migration, resulting in a lack of granulation and wound stasis. Wound edges may dry out and exposed soft tissue is no longer red and viable.

Healix Hydrogel is formulated with growth factors EGF and FGF to:
- Stimulate cell regeneration and division
- Promote fibroblast and keratinocyte migration
- Create a moist wound environment to maintain viable tissue and fresh skin edges
- Accelerate granulation tissue formation and epithelialization
- Improve wound contraction and complete closure
Healix Hydrogel – Unparalleled product exclusively for veterinary use, suitable for a range of clinical applications
Deep wounds such as:
- Traumatic wounds — bites, punctures, lacerations, degloving
- Medical wounds — post-surgery sites, penrose drain post-removal sites, wound dehiscence, bandage injuries and abrasions
- Chronic non-healing wounds — pressure sores, wounds in immunosuppressed and endocrine/diabetic cases, debilitated or geriatric animals
- Wounds of large surface area — burns, maggot wounds, sloughing, traffic accident/shearing injuries
Superficial wounds such as:
- Abrasions, minor cuts, scratches
- Ulcerated skin lesions

Advanced Cellular Regeneration
Corneal ulcers are commonly seen ophthalmic conditions in veterinary practice. Whether presenting as painful acute ulcers or difficult chronic non-healing ulcers, veterinarians aim for rapid control of infection and complete corneal repair. Apart from offering antibiotic eye drops, topical treatments are often limited to serum products. Research has shown that proteins such as EGF and IGF-1 contained in autologous serum may be the reason that therapy with serum has been successful in clinical studies on corneal healing. It has been found that EGF contained in serum is able to stimulate “proliferation of cultured epithelial cells and stromal fibroblasts” and “synthesis of fibronectin by epithelial cells”. 5

A long-anticipated innovative eye drop to improve treatment outcome for corneal ulcers and a welcome addition for your clinic in our current veterinary situation with limited topical treatment options.
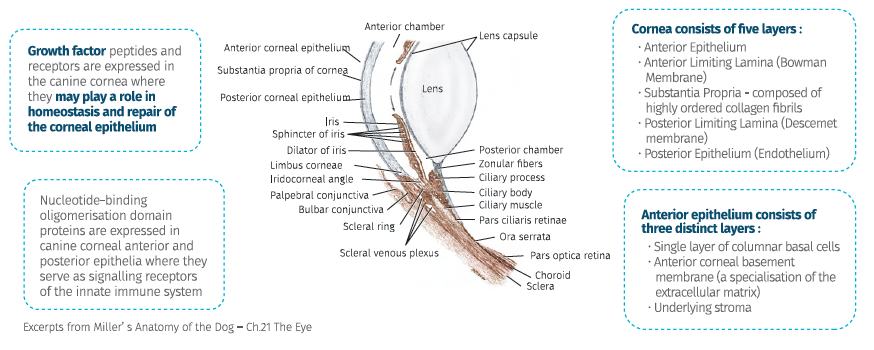
Scientific research in the recent decades have investigated the use of growth factor peptides to assist with the complicated process of corneal healing.
EGF and FGF have been of particular interest in their ability to stimulate cellular regeneration and corneal repair.6 EGF-like substance were identified in mouse tears and the addition of exogenous EGF were found to significantly improve healing of deep corneal ulcers in mice. 7 A randomised, double-blind, placebo-controlled multicentre clinical study in humans showed that EGF is effective in increasing the healing rate of traumatic corneal epithelial defects. 8 FGF along with EGF have been used in studies on bovine cornea and findings suggest these growth factors “stimulated the cell population as a whole” 9 and may “play key roles in corneal wound healing by regulating migration of corneal cells” 6 Various studies have also been carried out to investigate treatment of corneal ulcers using growth factors in rabbits, mice and primates. 10, 11

Healix Eye Drops offers a soothing easy-to-apply eye drop containing biofactors EGF and FGF to stimulate cellular regeneration
- EGF promotes division and differentiation of corneal epithelial and stromal cells, accelerating the synthesis of extracellular matrix (such as collagen and elastin) to facilitate repair of damaged ocular surface
- FGF helps maintain the health of ocular microvessels and enables the proliferation and chemotaxis of cell types involved in corneal recovery
- Convenient and readily available without need for venepuncture to obtain autologous serum for each patient
- Without the complications of serum storage
- Quality assurance and high purity
A long-anticipated innovative eye drop to improve treatment outcome for corneal ulcers and a welcome addition for your clinic in our current veterinary situation with limited topical treatment options.
- Mustoe TA, Pierce GF, Morishima C, Deuel TF. Growth factor-induced acceleration of tissue repair through direct and inductive activities in a rabbit dermal ulcer model. J Clin Invest. 1991 Feb;87(2):694-703. doi: 10.1172/JCI115048. PMID: 1991853; PMCID: PMC296361.
- Franklin JD, Lynch JB. Effects of topical applications of epidermal growth factor on wound healing. Experimental study on rabbit ears. Plast Reconstr Surg. 1979 Dec;64(6):766-70. doi: 10.1097/00006534-197912000-00003. PMID: 515226.
- Akane TANAKA, Toshiaki NAGATE, Hiroshi MATSUDA. Acceleration of Wound Healing by Gelatin Film Dressings with Epidermal Growth Factor. JVMS 2005; 67( 9): 909-913. DOI https://doi.org/10.1292/jvms.67.909
- Laato M, Heino J, Kähäri VM, Niinikoski J, Gerdin B. Epidermal growth factor (EGF) prevents methylprednisolone-induced inhibition of wound healing. J Surg Res. 1989 Oct;47(4):354-9. doi: 10.1016/0022-4804(89)90147-9. PMID: 2475671.
- Wirostko B, Rafii M, Sullivan DA, Morelli J, Ding J. Novel Therapy to Treat Corneal Epithelial Defects: A Hypothesis with Growth Hormone. Ocul Surf. 2015 Jul;13(3):204-212.e1. doi: 10.1016/j.jtos.2014.12.005. Epub 2015 Mar 28. PMID: 26045234; PMCID: PMC4498999.
- Grant MB, Khaw PT, Schultz GS, Adams JL, Shimizu RW. Effects of epidermal growth factor, fibroblast growth factor, and transforming growth factor-beta on corneal cell chemotaxis. Invest Ophthalmol Vis Sci. 1992 Nov;33(12):3292-301. PMID: 1428704.
- Tsutsumi O, Tsutsumi A, Oka T. Epidermal growth factor-like, corneal wound healing substance in mouse tears. J Clin Invest. 1988 Apr;81(4):1067-71. doi: 10.1172/JCI113418. PMID: 3258318; PMCID: PMC329632.
- Pastor JC, Calonge M. Epidermal growth factor and corneal wound healing. A multicenter study. Cornea. 1992 Jul;11(4):311-4. doi: 10.1097/00003226-199207000-00007. PMID: 1424650.
- Denis Gospodarowicz, Anthony L. Mescher, Charles R. Birdwell, Stimulation of corneal endothelial cell proliferation in vitro by fibroblast and epidermal growth factors, Experimental Eye Research, Volume 25, Issue 1, 1977, Pages 75-89, ISSN 0014-4835
- Frati, L., Daniele, S., Delogu, A., & Covelli, I. (1972). Selective binding of the epidermal growth factor and its specific effects on the epithelial cells of the cornea. Experimental Eye Research, 14(2). doi: 10.1016/0014-4835(72)90059-0
- Schultz G, Chegini N, Grant M, Khaw P, MacKay S. Effects of growth factors on corneal wound healing. Acta Ophthalmol Suppl. 1992;(202):60-6. doi: 10.1111/j.1755-3768.1992.tb02170.x. PMID: 1322013.
- Kovaléuka |, Murniece G. Normal reference ranges of ocular physiology and sonographic biometry of Latvian Hunting dogs. Vet World. 2019;13(4):807-81 1. doi:10.14202/vetworld.2020.807-811
- Williams D, Gimson L. Variation in intraocular pressure in the normal canine eye between different dog breeds. BSAVA Congress Proceedings 2020. 401 10.22233/9781910443774.65.3
- McLellan GJ, Miller PE. Feline glaucoma—a comprehensive review. Vet Ophthalmol. 2011;14 Suppl 1 (Suppl 1):15-29. doi:10.1111/j.1463-5224.2011.00912.x
- Oriá, Arianne & Filho, Emanoel & Raposo, Ana & Araujo, Nayone & Junior, Deusdete. (2015). Lacrimal production of cats: Schirmer Tear Test, Phenol Red Thread Tear Test and Endodontic Absorbent Paper Point. Enciclopédia Biosfera. 2085-209110.18677/Enciclopedia_Biosfera_2015_182.
Email: info@ambrosia-global.com
Tel.: +852 2866 8328
Sales Representative
David Man
Mobile: +852 91995079
©All rights reserved

